Epidurals: what you need to know
An epidural is an injection in your back that can stop the pain of the contractions during your baby’s birth. There are a few risks and side-effects to consider, but epidurals are considered safe and effective, and 1 in 3 women in labour choose to have one.
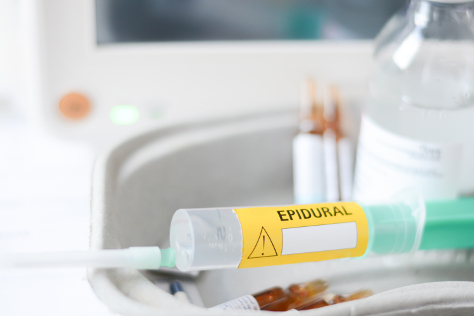
What is an epidural?
It’s when anaesthetic medicine is injected into the part of your spine called the ‘epidural space'. This blocks the pain of your contractions by numbing the nerves around your lower abdomen. How numb you get depends on the combination of drugs the anaesthetist uses and how strong the dose.
Epidurals have been considered a safe and effective form of pain-relief in childbirth for many years: one in three women choose to have one – and 90% find it effective.
How is an epidural given?
It sounds a bit alarming when described in detail, but as you’ll be having it during a pretty full-on time in labour, you probably won’t be particularly bothered by that point!
Basically, the anaesthetist (the only person qualified to give an epidural) inserts a hollow needle into the epidural space in your lower back, usually while you are sitting down and leaning forward (staying as still as possible). A fine tube is then put through the needle, which is pulled out once the tube is in place. The anaesthetic is delivered through the tube, and you should feel the effects about 20 minutes later.
You’ll also be connected to a drip via a cannula (tube) in your hand in case you need drugs to raise your blood pressure, and your baby will also be constantly monitored, so there will be a lot of tubes and equipment about and you won’t be as mobile. Your blood pressure will be checked every few minutes, too.
How will I feel?
If the tube is in the right place (sometimes the anaesthetist will have to adjust it or start again) you should feel complete relief from pain. The idea is to leave you with enough feeling so you can push the baby out when the time comes, but if it’s worked too well you may feel numb all the way down your legs! Sometimes it only works partially, so you may still have some pain in your abdomen. Top-ups of the pain-relieving drugs can usually be given by the midwife once the tube is in place.
Many hospitals make you stay in bed after you’ve had an epidural, but some offer a ‘mobile epidural’ which involves a lower dose of the drugs. The advantage of this is you can still walk around and have an active birth.
When can I have an epidural?
You can have an epidural at any time from the beginning of labour, but most women who choose one have it when they’re around 5cm dilated, when contractions get more intense and painful.
If you ask for one very late in labour – at 8 or 9cms dilated – your midwife may advise against it because you’re so nearly there and there’s a chance the epidural will slow the labour down.
What are the risks and side-effects of an epidural?
It’s considered a safe form of pain-relief: the NHS says the risk of permanent harm is between 1 in 80,000 and 1 in 320,000. But there are some possible downsides:
- You may feel sick, dizzy or shivery because your blood pressure has fallen. Some women report feeling intensely itchy
- Sometimes it can take a couple of goes to get the needle and tube in exactly the right place, which can be stressful
- Epidurals are associated with a longer second stage of labour and an increased chance of needing an assisted delivery with forceps or ventouse
- Because you may not feel when you need to pass urine, you could have a catheter in your bladder. All those tubes plus the baby’s monitoring equipment can feel like the birth is passing out of your control
- You’re less likely to be able to walk about and have an active birth, which is the best way to ensure the baby is in the right position
- Some women get a severe headache for several days afterwards, which is caused by some spinal fluid leaking out when the needle is removed. This is quite rare and happens in only one in 100 cases
- You can get epidurals in doctor-led units but not midwife-led ones or during home births.